Jan 2, 2025
Mental Health
Featured
Understanding the Complexity of Mental Health

Introduction
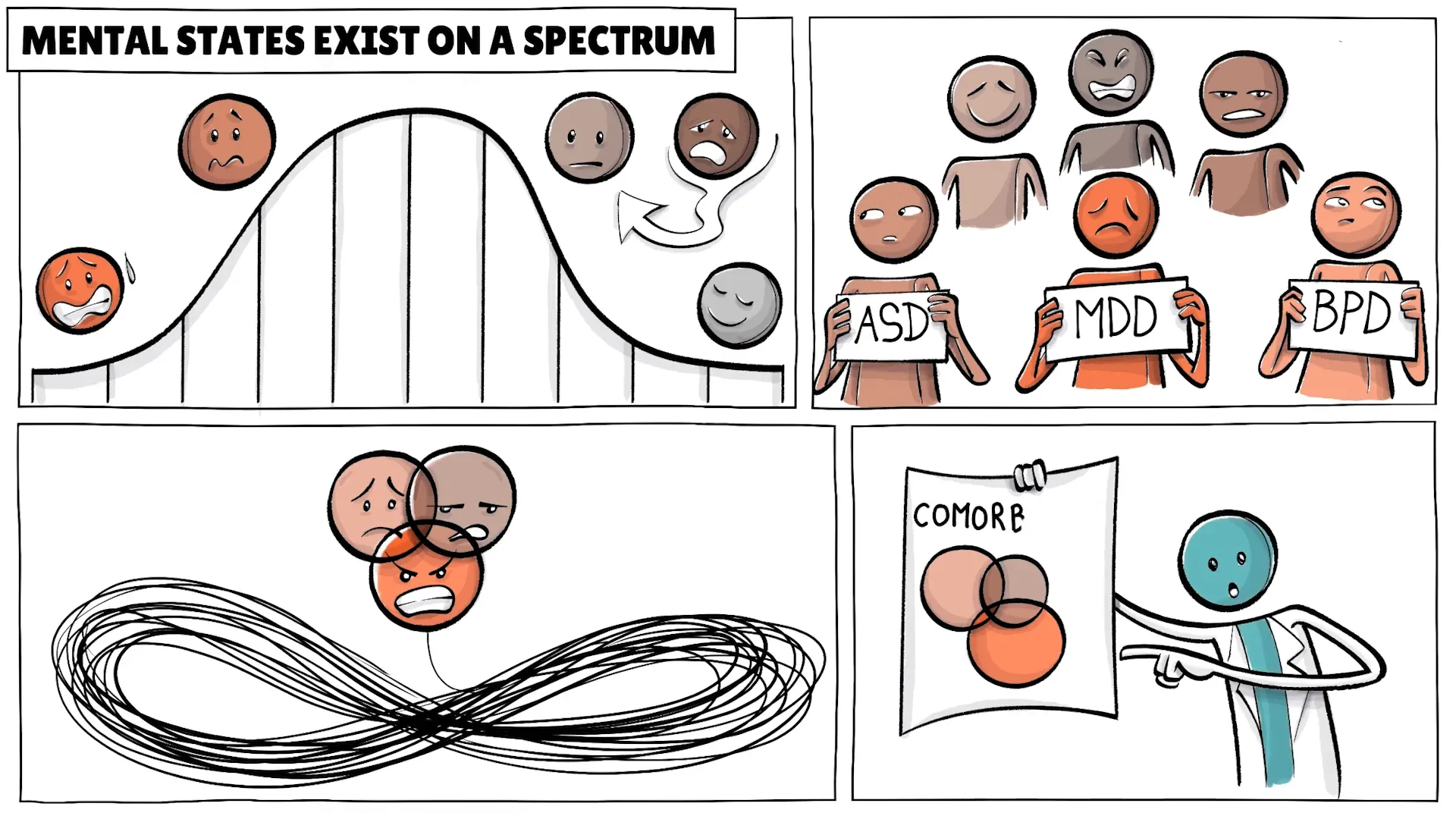
Mental health is a nuanced and intricate subject that transcends simple categorizations. It exists on a spectrum and is influenced by a myriad of factors, including genetics, environment, and personal experiences. Understanding the complexities of mental health is crucial for both individuals and healthcare providers, as it informs diagnosis, treatment, and societal perceptions.
Complexity of Mental Health
Imagine not being entirely calm or anxious, but existing somewhere in between, perhaps feeling tired or distracted. This illustrates how all mental states, such as Autism Spectrum Disorder, Borderline Personality Disorder, or Major Depressive Disorder, exist on a spectrum. Each condition has numerous variations, many overlapping with others, resulting in what is known as comorbidity.
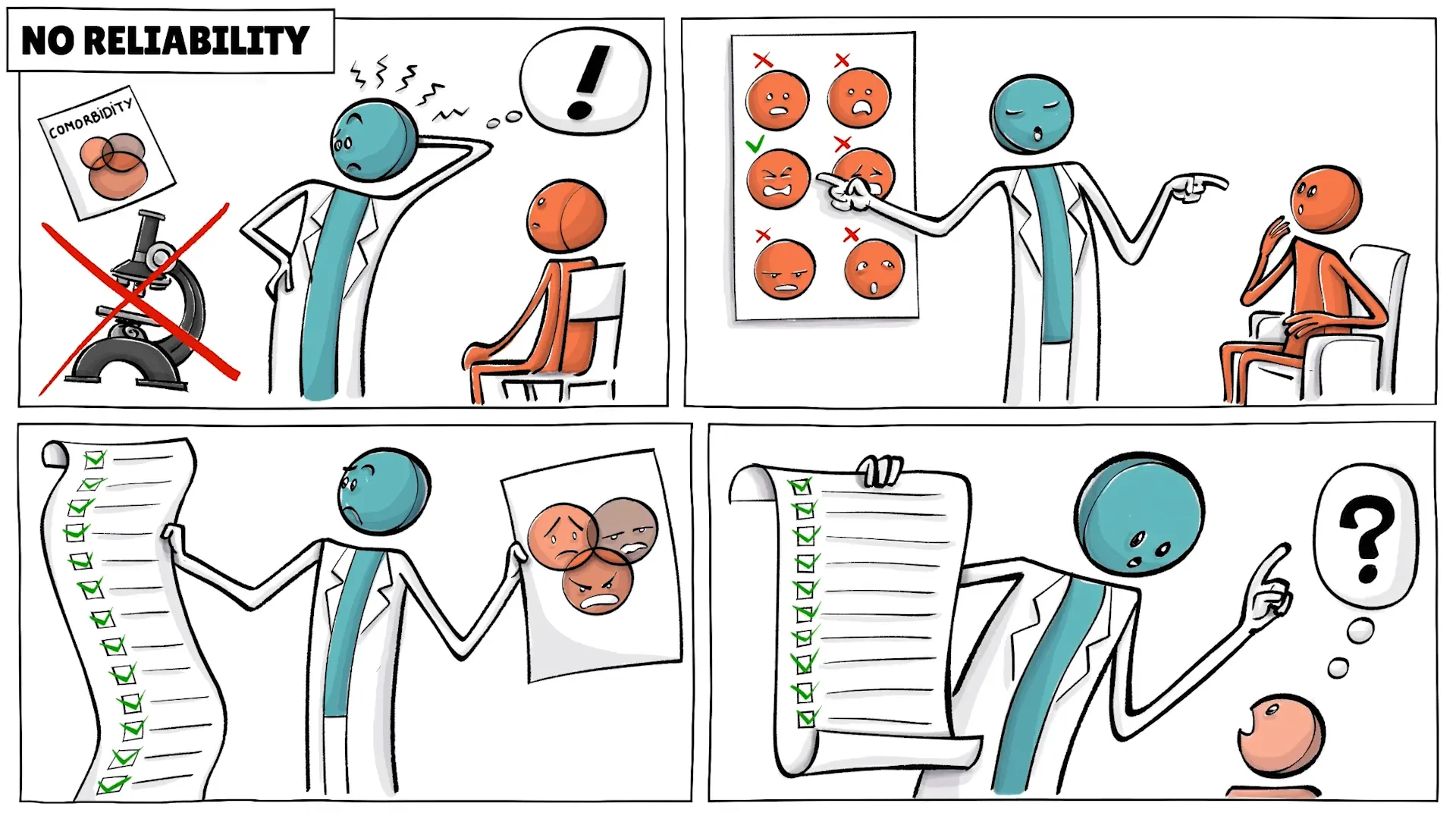
Unlike a straightforward injury like a broken leg, mental health issues are rooted in highly complex origins. For instance, schizophrenia may have a strong genetic component, while anxiety can stem from various factors, including genetic traits and childhood trauma. Moreover, most mental disorders lack clear biomarkers, which complicates diagnosis and treatment.
Diagnostic Manuals
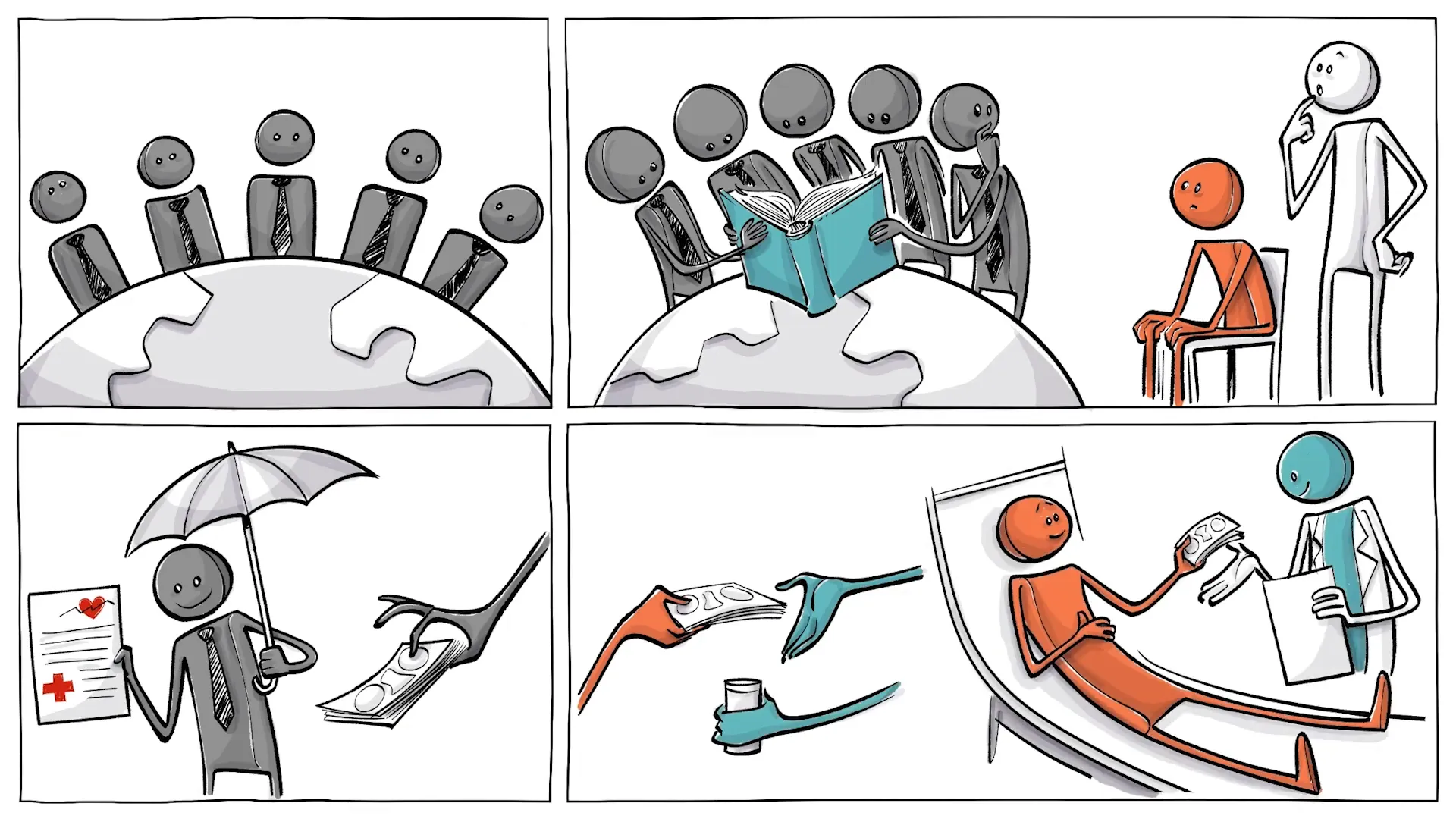
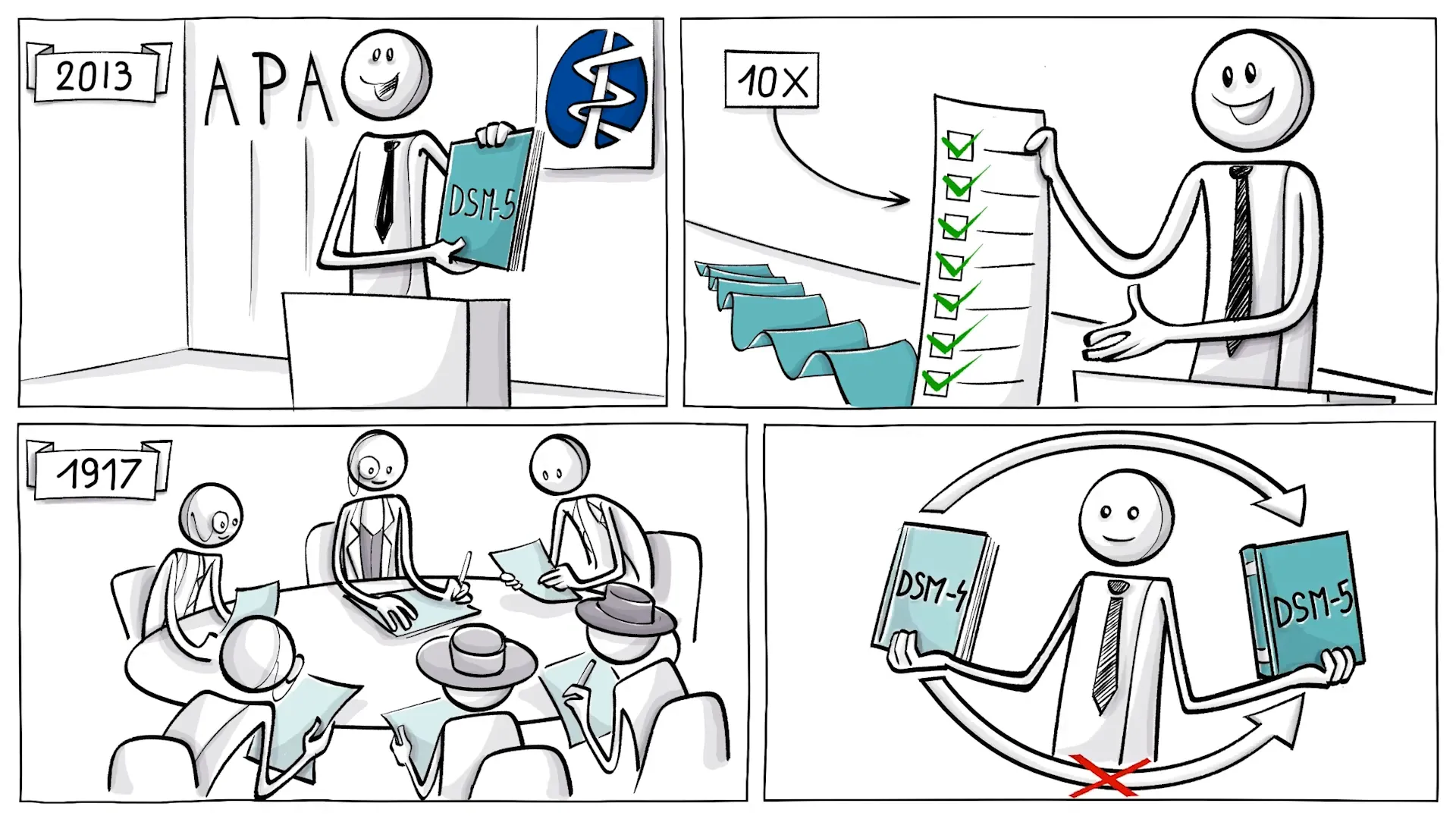
To navigate this complexity, psychiatrists rely on diagnostic manuals. In the U.S. and Australia, the Diagnostic and Statistical Manual (DSM) is the primary guide, while the International Classification of Diseases (ICD) is used globally. These manuals help clinicians categorize mental health conditions and establish a common language for discussing symptoms and treatments.
Historically, these manuals have evolved. For example, homosexuality was once classified as a sociopathic personality disturbance but was removed as a mental disorder in 1974. Such changes reflect shifting societal norms and scientific understanding.

The Societal and Medical Influence
The influence of these manuals extends beyond clinical settings to societal perceptions and health policies. They help determine who is considered mentally ill and what treatments are covered by public health insurance. For instance, a significant number of teenage girls in the U.S. are prescribed antidepressants, raising questions about the criteria used for such diagnoses.
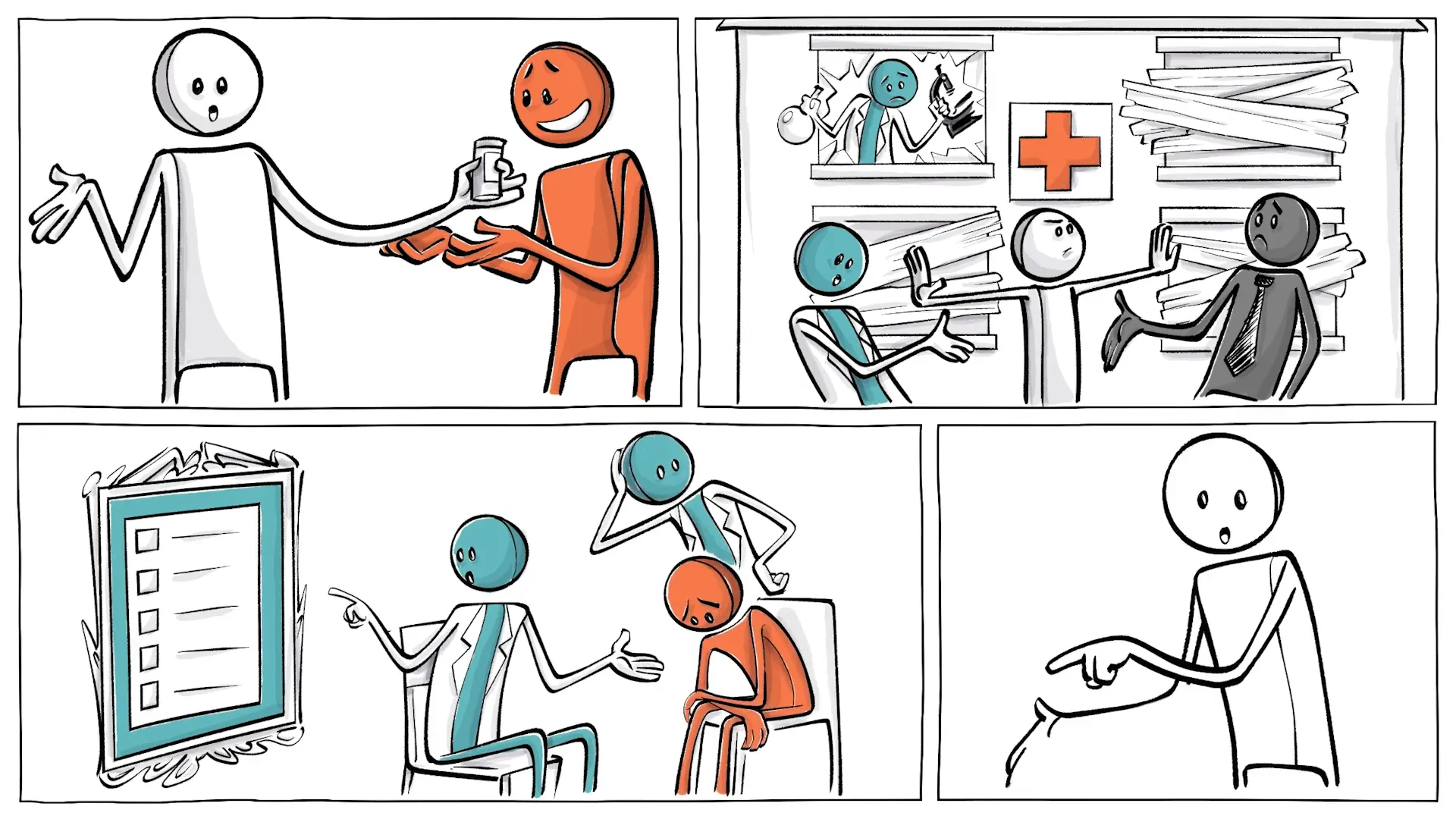
The lack of clear biological evidence in mental health diagnoses leads to reliance on subjective assessments, which can vary widely among practitioners. This subjectivity can result in misdiagnoses, especially in children who may not have the language skills to articulate their feelings accurately.
Subjective Diagnosis
Psychiatrists often depend on what they observe, self-reports from patients, standardized tests, and input from family members. However, the overlap of comorbidities complicates this process, making it challenging to pinpoint a specific disorder among many that share similar symptoms.
For example, an autistic child may struggle with routines due to a need for predictability, while a child with ADHD may thrive on novelty. A child exhibiting traits of both could become confused and misdiagnosed, illustrating the challenges of subjective diagnosis.
Combination of Comorbidities
The interplay of different mental health conditions can create a convoluted clinical picture. This complexity is exacerbated by the fact that diagnostic criteria can change over time, leading to an ever-expanding list of recognized disorders. For instance, the DSM-5 published in 2013 includes 297 disorders, a significant increase from previous editions.
As awareness and understanding of mental health evolve, so too do the definitions and classifications within these manuals. This evolution can lead to what’s termed "diagnostic inflation," where conditions that may have once been considered normal variations of behavior are now classified as disorders.
Other Challenges
The challenges in diagnosing mental health conditions are not limited to the manuals themselves. There are societal pressures, stigmas, and biases that influence how conditions are perceived and treated. For example, grief from losing a loved one can now be classified as Major Depression Disorder, leading to potentially unnecessary medication.
Additionally, the introduction of new disorders, such as Disruptive Mood Dysregulation Disorder, raises concerns about the medicalization of normal childhood behavior, like tantrums or outbursts.

DSM-5 Overview
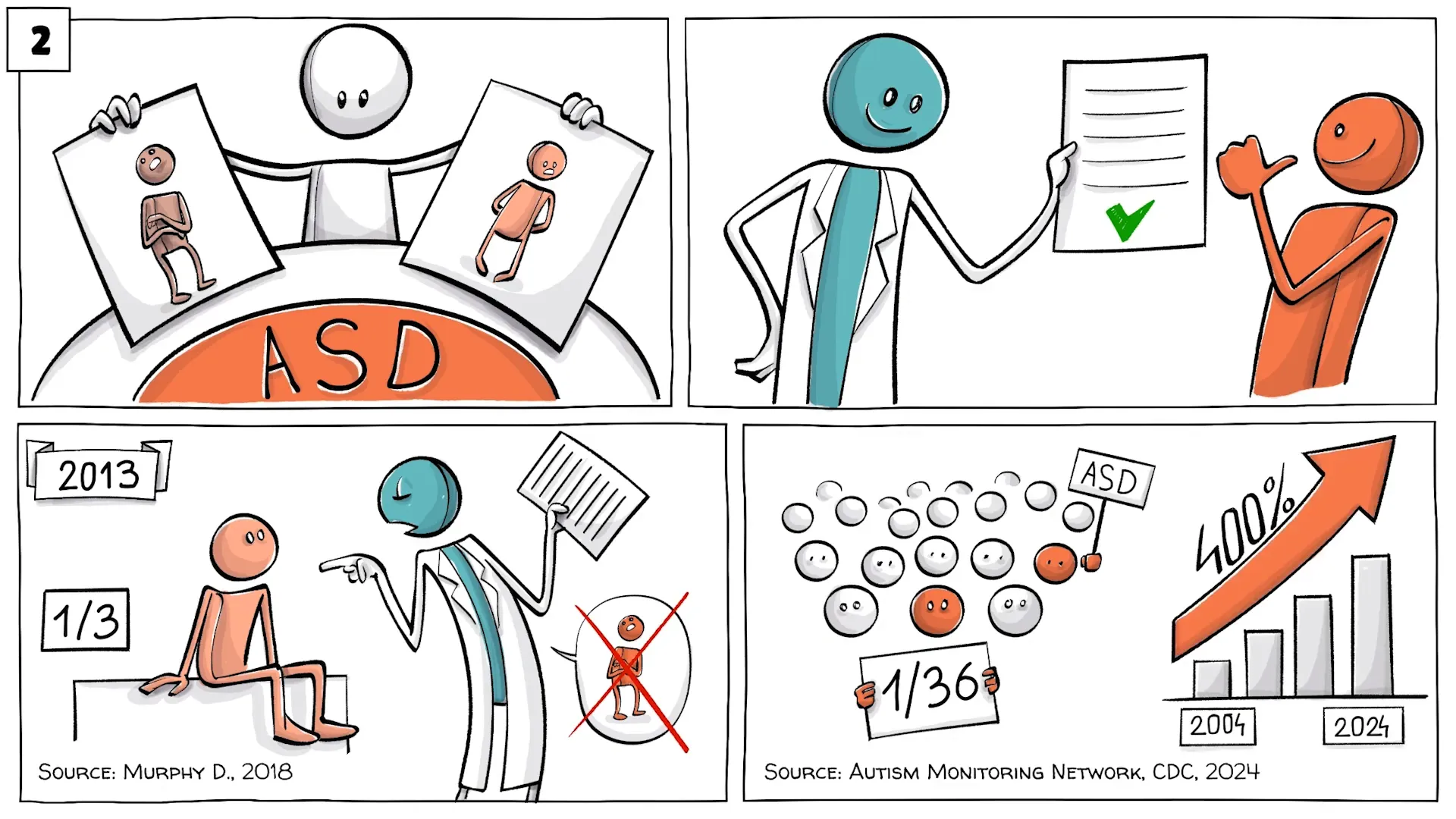
The DSM-5’s publication marked a significant shift in the landscape of mental health diagnosis. It not only expanded the number of recognized disorders but also altered existing definitions. For example, the merging of Autism and Asperger's Syndrome into Autism Spectrum Disorder (ASD) increased the likelihood of diagnosis, but also led to confusion regarding the criteria.
Today, approximately 1 in 36 children in the U.S. are diagnosed with ASD, a staggering increase from 20 years ago. Such statistics highlight the impact of diagnostic changes on public perception and healthcare practices.
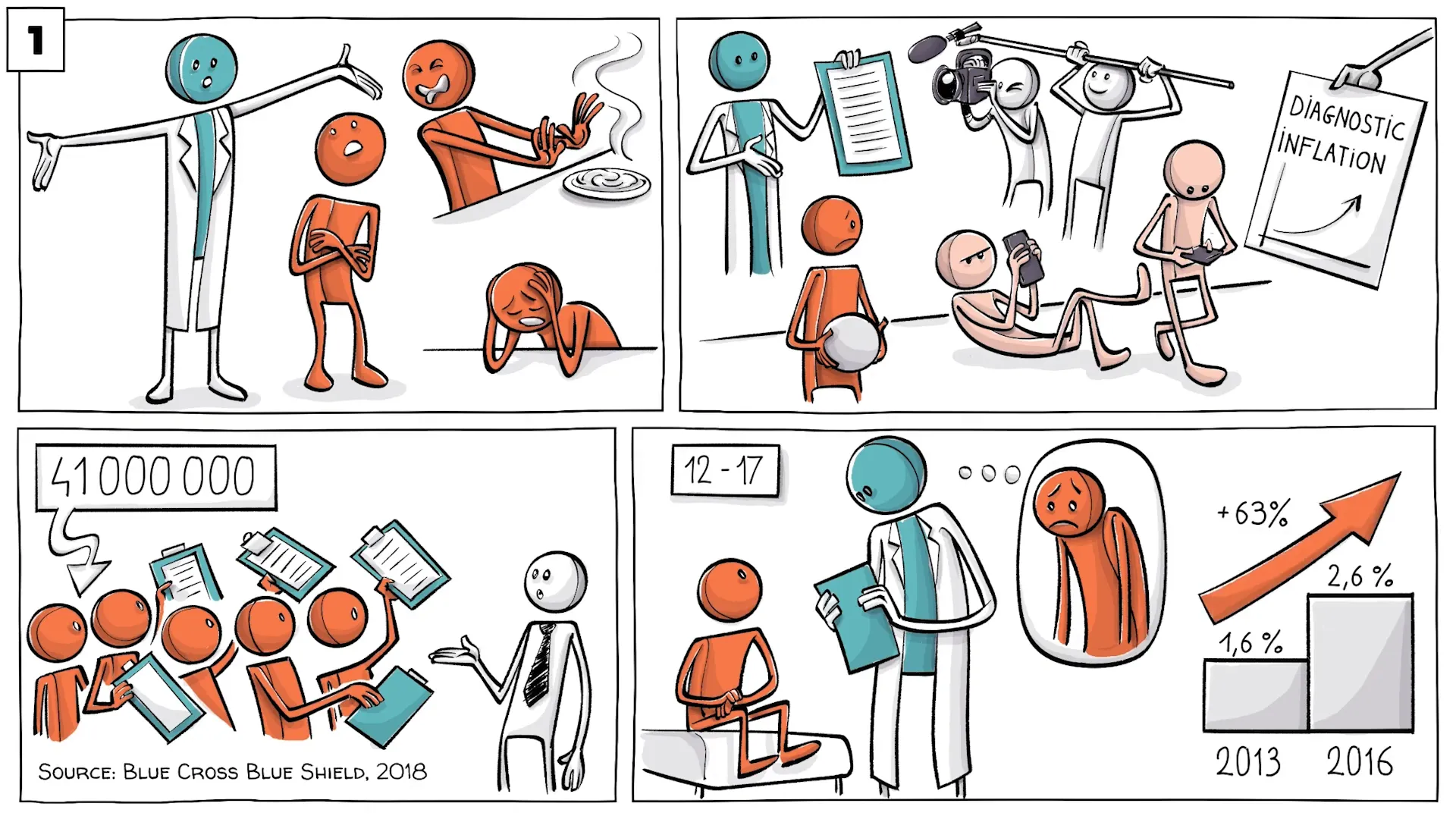
Diagnostic Inflation
Diagnostic inflation has become a pressing concern in the mental health community. For instance, the rate of major depression diagnoses in adolescents surged from 1.6% in 2013 to 2.6% in 2016. This 63% increase prompts questions about the criteria being used and the implications for treatment.
As definitions broaden and awareness increases, it is essential to assess whether the rise in diagnoses reflects genuine increases in mental health issues or if it is a result of changing criteria.
Autism Redefined
The redefinition of autism in the DSM-5, which combined Autism and Asperger's Syndrome into one category, has significant implications for diagnosis and treatment. While it aims to create a more cohesive understanding of the spectrum, it also means that many individuals who previously identified with Asperger’s may not fit neatly into the new criteria.
This change raises concerns about underdiagnosis and the potential for individuals to miss out on necessary support and resources.
Grief Diagnosis
The classification of grief as a mental disorder has sparked heated debates. The DSM-5 allows for grief to be diagnosed as Major Depression Disorder, which can lead to treatment with medication. This pathologization of a natural emotional response raises ethical questions about the appropriateness of such diagnoses.
Many believe that experiencing deep sadness after a loss is a normal human reaction and that labeling it as a disorder can undermine the validity of that grief.

Mood Disorders
Mood disorders encompass a range of conditions, including depression and bipolar disorder. The challenge lies in accurately diagnosing these disorders, especially since symptoms can vary widely between individuals. Moreover, the criteria for mood disorders can sometimes overlap with other mental health conditions, complicating the diagnostic process.
As the understanding of mood disorders evolves, it remains crucial to differentiate between genuine disorders and normal emotional fluctuations.

ADHD Challenges
Attention-Deficit/Hyperactivity Disorder (ADHD) presents unique challenges, particularly in how it is diagnosed. Historically studied primarily in boys, the diagnostic criteria often fail to capture how girls and adults experience ADHD, leading to misdiagnoses and inappropriate treatments.
This oversight can result in women being misdiagnosed with conditions like bipolar disorder, demonstrating the need for more inclusive diagnostic criteria that account for diverse presentations of ADHD.
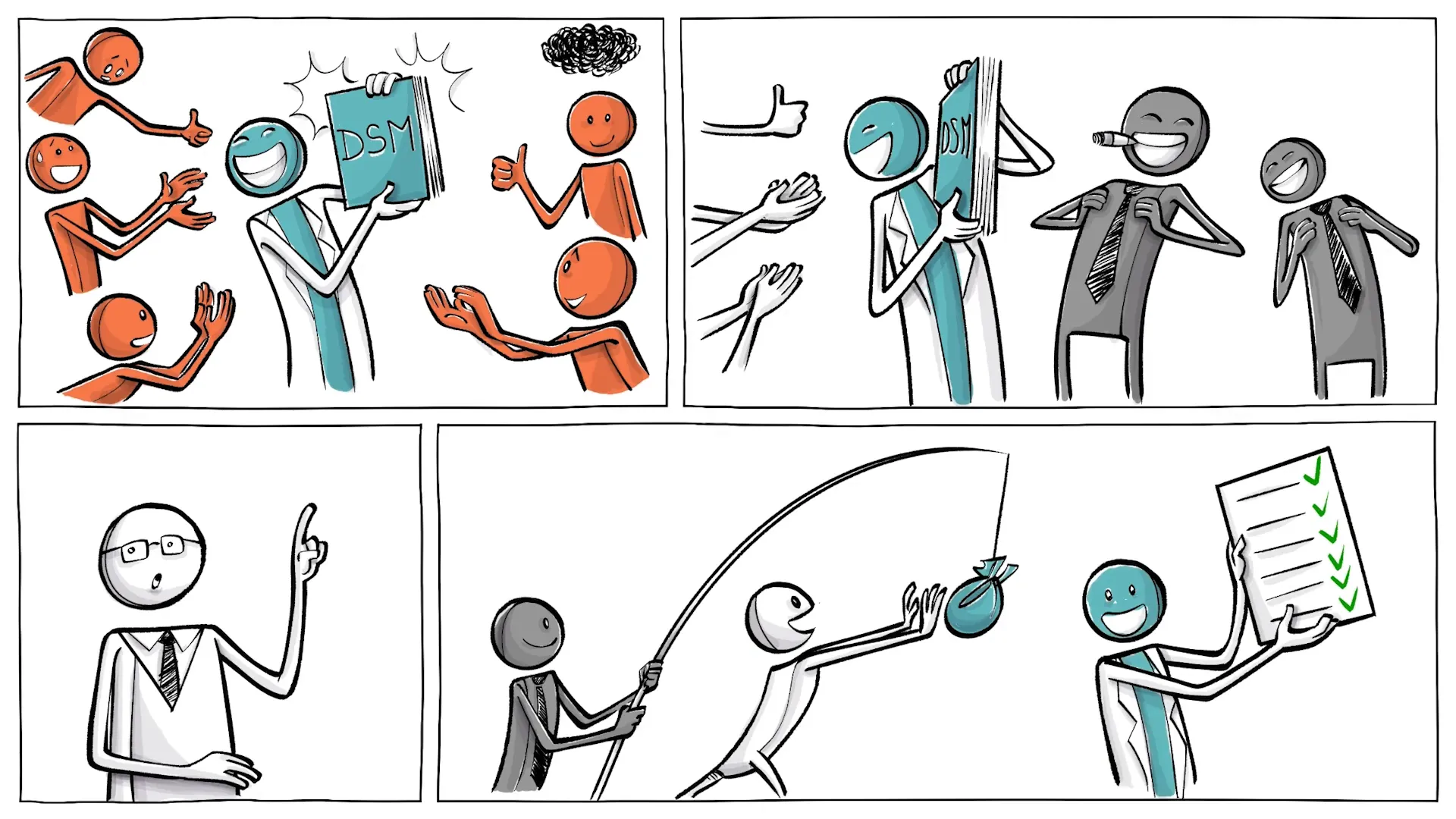
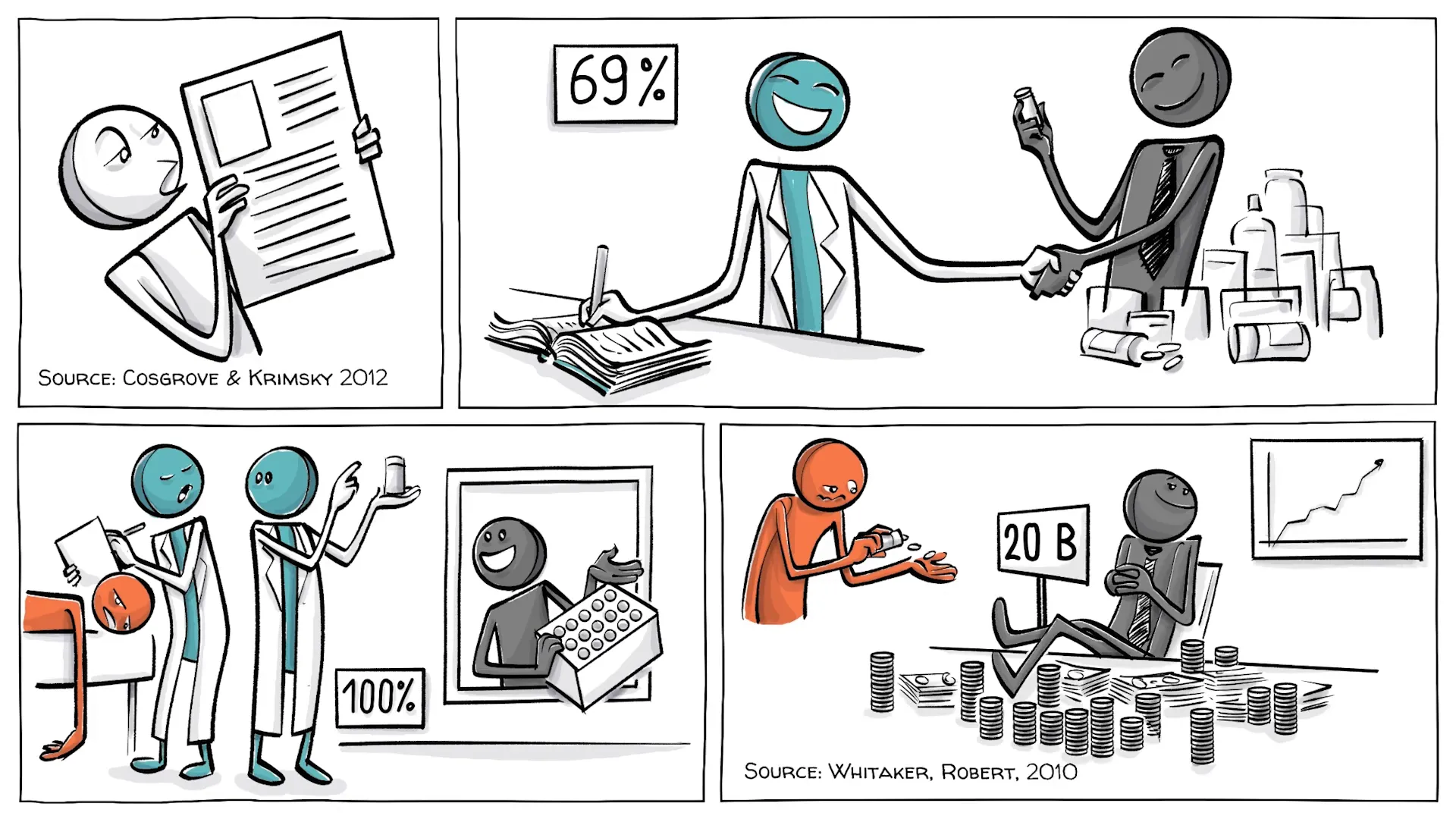
Who Benefits
While many patients benefit from the advancements in mental health diagnosis and treatment, it is vital to scrutinize who else may gain from these changes. The DSM is produced by the American Psychiatric Association, whose members are both authors and users of the manual, raising potential conflicts of interest.
This relationship can lead to questions about the motivations behind certain diagnoses and treatments, particularly when pharmaceutical companies become involved.
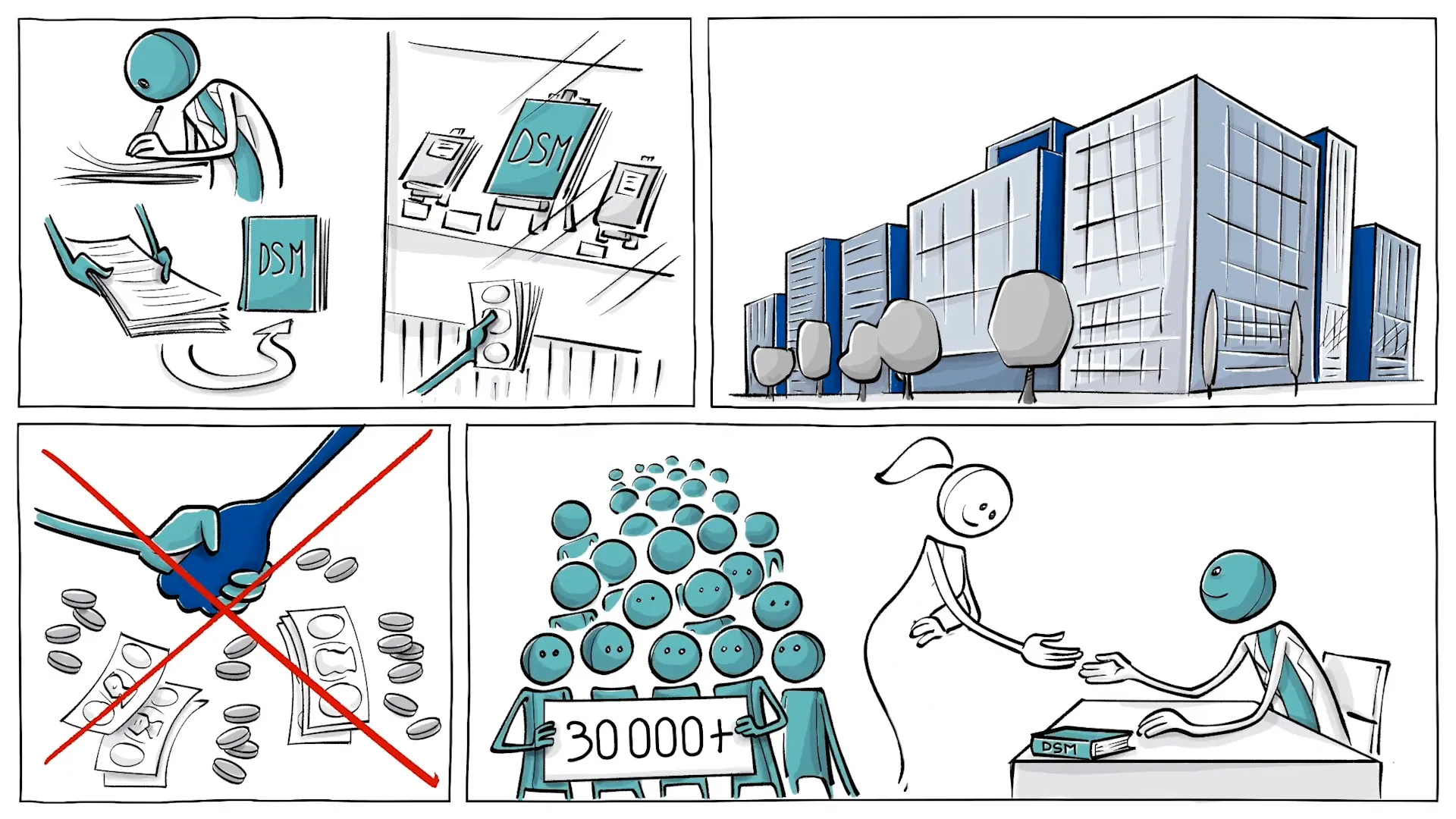
Collaborative History
The collaboration between psychiatrists and pharmaceutical companies has deep historical roots. Beginning in the mid-20th century, this relationship has evolved into a partnership that seeks to address mental health issues but may also lead to conflicts of interest.
With the rise of antidepressants in the 1950s, the bond between mental health professionals and drug manufacturers strengthened, resulting in significant influence over treatment options and public health policies.
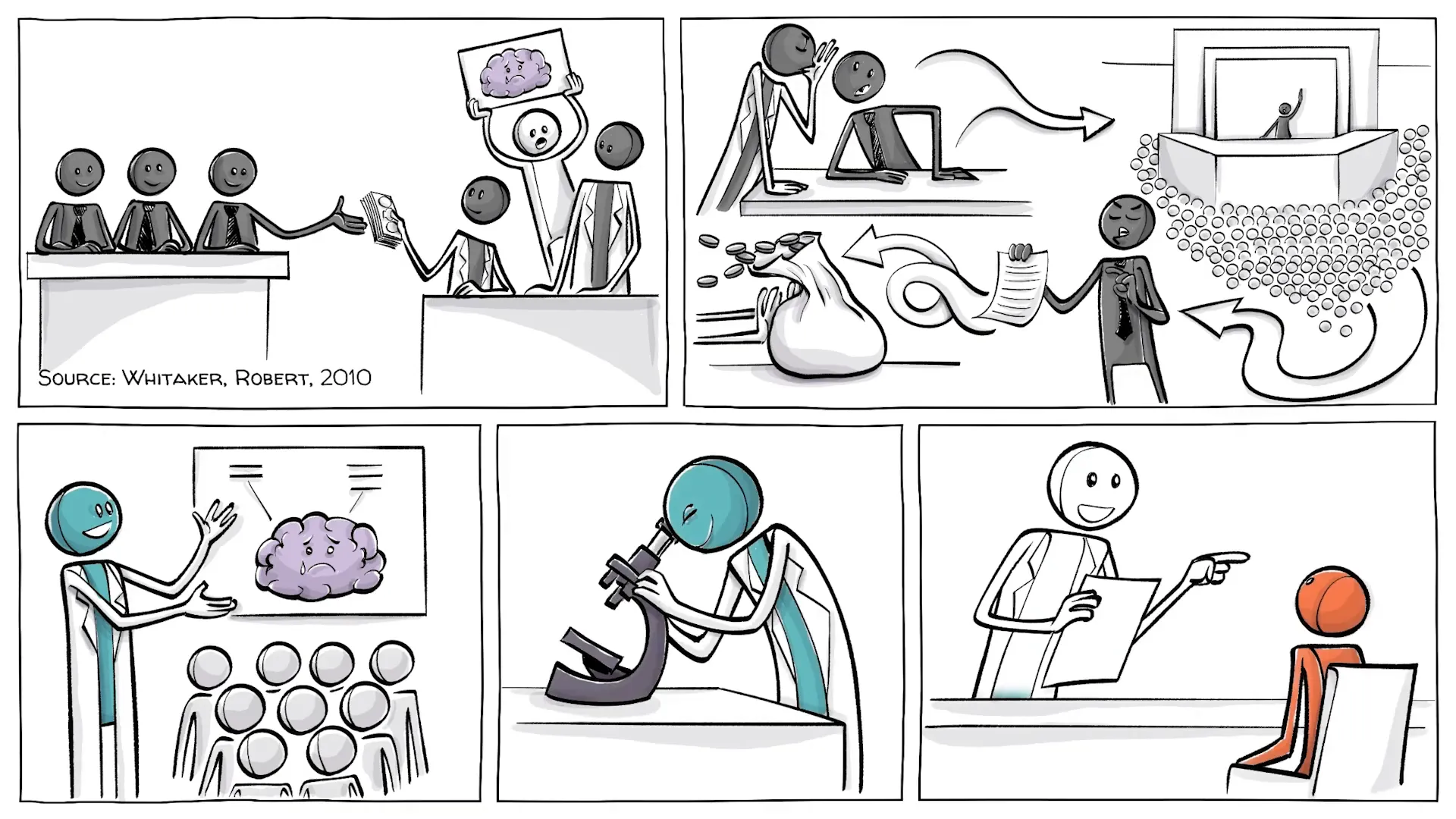
Pharmaceutical Influence
Pharmaceutical companies play a substantial role in shaping mental health treatment. With significant funding directed towards awareness and research, their influence extends into how mental health conditions are perceived and treated.
For instance, a congressional investigation revealed that a considerable portion of the American Psychiatric Association's budget comes from pharmaceutical companies. This financial backing raises concerns about the integrity of the DSM and the motivations behind certain diagnoses.
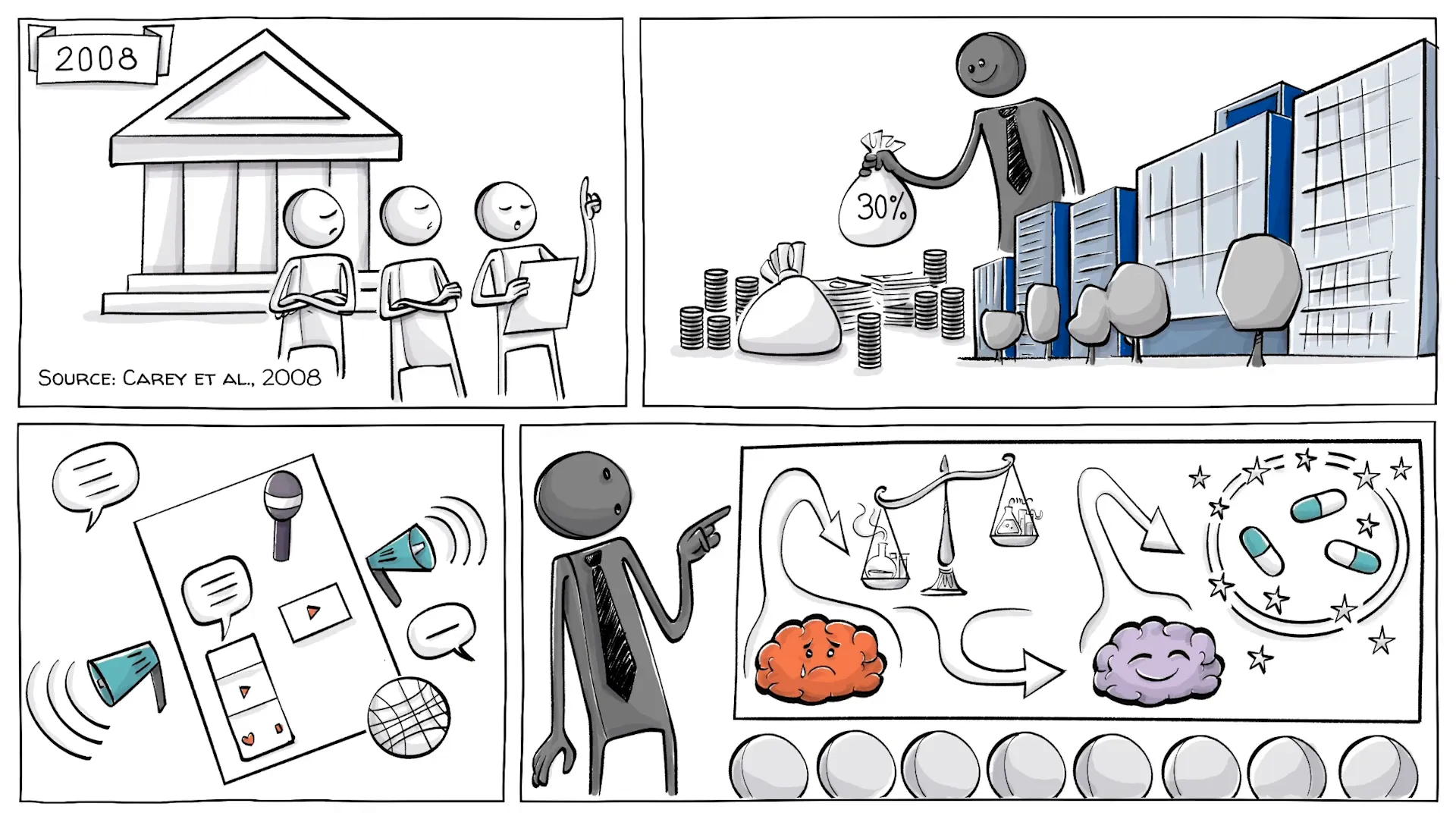
Doctor Connections
The connections between the DSM’s authors and pharmaceutical companies are striking. A notable percentage of doctors involved in creating the DSM-5 had financial ties to these companies, particularly in areas where medication is a primary treatment.
This overlap raises questions about the objectivity of the DSM and whether it adequately serves the best interests of patients or the pharmaceutical industry.
What Do You Think?
The complexities of mental health diagnosis and treatment prompt many questions. How can conflicts of interest be mitigated without stifling essential research? Is it possible to develop guidelines that respect the complexities of mental health while ensuring effective treatment?
Engaging in these discussions is vital for advancing mental health care and ensuring that patients receive the best possible support.
Conclusion
The complexities of mental health are multifaceted, requiring a thoughtful approach to diagnosis and treatment. As we continue to explore these issues, it’s essential to engage in conversations that challenge existing paradigms and promote understanding.
Thank you for joining us on this journey to better comprehend mental health and its implications for individuals and society at large.
This article was created from the video Are We All Soon Officially Nuts? with the help of AI. It was reviewed and edited by a human.



